Endodontic treatment
Endodontic treatment is a complex process of diagnostic, preventative, and therapeutic procedures aimed at removing the infection from the root canal and surrounding periodontal tissues. Endodontic treatment methods always aim at preserving as much of the tooth as possible.
- Causes of root infection
- Endodontic treatment stages
- Endodontic retreatment
- The dangers of untreated pulpitis
- Does tooth root canal treatment hurt?
- Tooth restoration after endodontic treatment
- Endodontic treatment with dental microscope
- Which is better – to treat infected dental canals or get an implant?
- Endodontic treatment in our clinic
- Pricelist
Causes of root infection
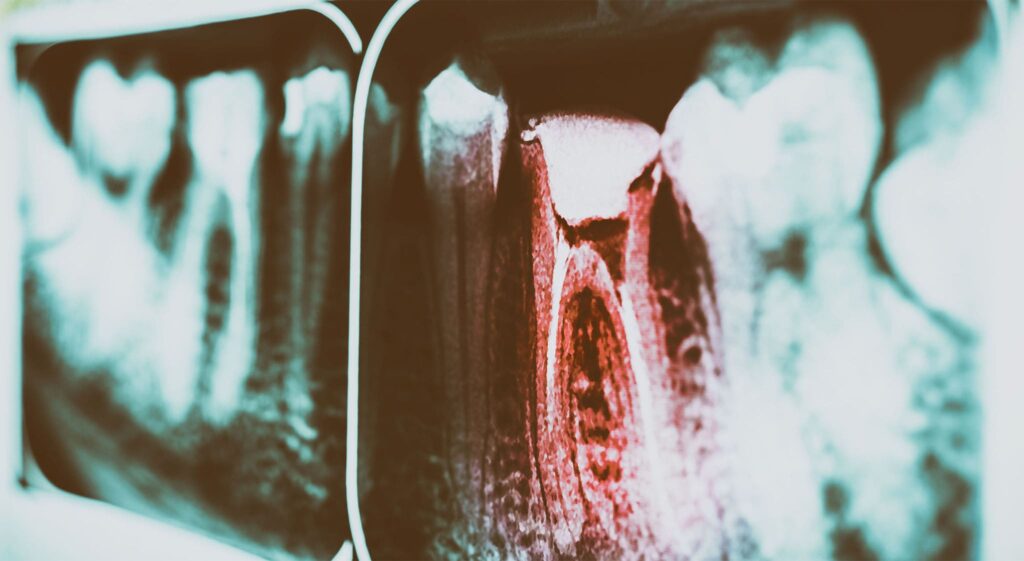
Pulpitis
In addition to a hard outer layer, the tooth also has a soft inside called the pulp. The pulp consists of blood vessels and nerve clusters that provide nutrition and ensure the regeneration of the other components of the tooth. A healthy pulp is protected from infections by the enamel and the internal tooth tissue called dentin.
Prolonged tooth decay may damage the protective layers of enamel and cause pulpitis. Dental pulpitis is the inflammation of the inside of the tooth that begins when an infection enters the pulp.
The main causes of pulpitis:
- Untreated tooth decay, accompanied by the formation of a deep infected cavity that reaches the pulp of the tooth, is the most common cause of dental pulpitis and can be prevented with proper oral hygiene and regular dental check-ups.
- Poor dental treatment: damage to the pulp chamber with dental instruments; careless drilling before dental filling; use of poor-quality filling materials; improper filling method.
- Tooth cracks and other injuries.
- Tooth wear caused by various dental diseases.
- Gum diseases, such as gingivitis and periodontitis. Poor periodontal treatment resulting in infection of the dental pulp.
- Long-term destructive effects of chemicals, overheating or overcooling.
Pulpitis types and symptoms
Like many other dental diseases, pulpitis can present as an acute or chronic illness. Both types are divided into several subtypes, depending on the localization of the pathology and the severity of the disease:
- Acute pulpitis occurs suddenly and is followed by severe pain. It usually occurs as a result of prolonged tooth decay or trauma. The pain intensifies at night and only disappears after taking painkillers.
Acute pulpitis occurs in two stages:- Focal pulpitis – lasts about 2 days and is characterised by periodic acute pain. The pain can last up to half an hour and recur every few hours. In focal pulpitis, the infection damages part of the nerve, so the pain is localised only in the area of the affected tooth.
- Generalised pulpitis – normally begins on the third day of the disease, when the infection spreads throughout the dental pulp. Generalised pulpitis is characterised by a pulsating pain that spreads throughout the jaw. Abscesses may form in the mouth due to generalised pulpitis, which in turn may cause headaches and an increase in body temperature.
- Chronic pulpitis develops as a consequence of untreated acute pulpitis. In the chronic form of pulpitis, the severity of the symptoms disappears, and the sharp pain changes to periodic. Untreated chronic pulpitis lasts up to one year and progresses in several stages:
- Fibrous pulpitis – the most common type of chronic pulpitis. It is characterised by the proliferation of fibrous tissues in the pulp chamber. At this stage, tooth enamel changes in colour, bad breath appears, and tooth sensitivity increases.
- Pulp necrosis – untreated fibrous pulpitis can turn into a necrotic form that progresses into the coronal part of the pulp. At this stage of the disease, the nerves in the pulp begin to die.
- Hyperplastic pulpitis – a granular tumour is formed in the pulp chamber, occupying the root of the tooth and the coronal part of the pulp. Touching a tooth damaged by hyperplastic pulpitis causes severe pain and bleeding.
Treatment of pulpitis
In order to eliminate infection, inflammation, and pain caused by pulpitis and to preserve the tooth, it is necessary that we perform endodontic treatment of the damaged tooth. There are two main methods used to treat pulpitis, the choice of which depends on the cause, stage, and type of the disease:
- Conservative treatment methods are used in the cases of a slight infection, before the inflammatory process has begun in the pulp. The treatment process is almost the same as for caries, but more attention is being paid to anti-inflammatory medications. Disinfectants are used to treat the damaged pulp, which stops the bacteria and contributes to the regeneration of the affected tissues. A temporary dental filling is then applied, to allow further treatment if this method fails. The patient has the temporary filling for several days until the inflammation stops, which is when the tooth is filled permanently.
- Surgical treatment of pulpitis involves the partial or complete removal (depulpation) of the damaged pulp. In this case, the root canals of the tooth are deeply cleaned and then filled with a special substance. Depending on the shape of the pulpitis, its surgical treatment can be performed over either one or several visits.
Endodontic treatment stages
1 – Oral inspection and diagnosis

To assess the extent of tissue damage and the overall clinical situation, the endodontist applies a set of diagnostic methods which include: interviewing the patient; inspecting the patient’s mouth, using dental probes and other special instruments; Radiological examinations, to make an accurate diagnosis and locate the root canals.
2 – Creation of the treatment plan

From analysing the diagnostic test results, the endodontist is able to get a comprehensive idea of the clinical situation. The dentist compares the prognosis for different treatment options, determines the optimal treatment method, drafts a plan for the most effective treatment method, and discusses it with the patient.
3 – Preparation for the procedure

Preparation for endodontic treatment may include:
- Treatment of periodontal diseases.
- Filling of decay-damaged teeth.
- Restoration of the worn teeth.
- Removal of crown prostheses if they are installed on the causative tooth.
- The patient gets some form of anaesthesia before the procedure.
4 – Tooth root canal treatment

Endodontic treatment is performed in three main steps:
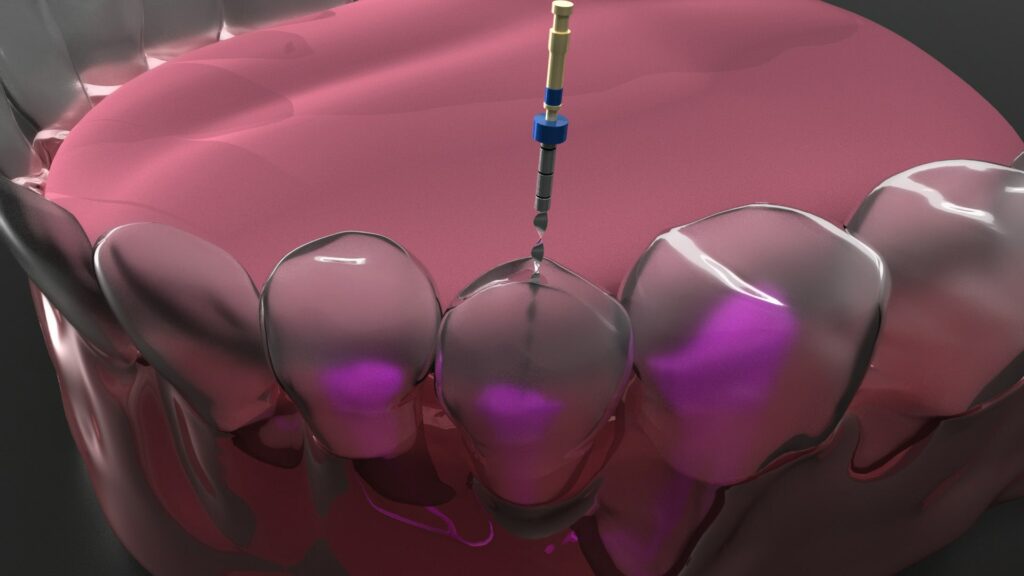
- Accessing the tooth root canals – locating and forming an entrance to the canals that allows endodontic instruments to be inserted.
- Treatment of tooth root canals– thorough removal of damaged tissues and disinfection of the infected dental canals using special instruments, medications, and other necessary equipment such as root tip locator, endodontic microscope, etc.
- Filling the canals – filling the root canals with special highly-resistant dental substances called gutta-percha pins. X-ray control of the quality of the canal closure is performed, and a temporary dental filling is placed.
5 – Restoration of tooth shape and function

The choice of tooth restoration method is very important to ensure a successful treatment outcome. The most common method of restoration is with a filling. In modern dentistry, endodontically treated teeth also receive restored crowns (when more than 50% of the tooth is damaged) or ceramic overlays (if the tooth is fairly well preserved). Teeth must be restored no later than 2 weeks after endodontic treatment.
Endodontic retreatment
A tooth that has undergone endodontic treatment is left for observation and if unsuccessful may require retreatment.
The failure of primary endodontic treatment is almost always associated with bacterial entry into the root canal system, caused by poor oral hygiene. In addition, endodontic retreatment may be required if the tooth does not recover after the initial treatment for physiological reasons, or if the treatment has been performing poorly.
Less common causes of endodontic retreatment include the formation of cysts, inflammation of bone tissues, poor immunity, comorbidities from the patient, the patient’s reaction to foreign bodies, damage to bone and connective tissue healing sites.
Modern endodontic hardware increases the chances of a successful initial endodontic treatment. By performing treatment with a trusted specialist, the patient can help to avoid serious complications of the procedure.
The dangers of untreated pulpitis
Chronic pulpitis can cause severe toothache and headaches as well as provoke serious health complications, including periodontitis, osteomyelitis, trigeminal neuritis, and more. In the most severe cases, untreated pulpitis can lead to sepsis and death.
Therefore it is highly recommended that you consult an endodontist immediately after feeling the first symptoms of pulpitis. This ensures a timely professional diagnosis and helps you avoid any serious complications.
Does tooth root canal treatment hurt?
Treatment of the root canals is not painful as the patient receives local anaesthesia before the procedure. In severe cases, or when multiple teeth need to be treated, endodontic treatment may be performed under general anaesthesia.
Tooth restoration after endodontic treatment
It is impossible to restore lost nerves and blood vessels of the teeth, and the structure of the teeth inevitably weakens after their loss. Therefore, tooth restoration is especially important during endodontic restoration. The main methods of restoring the shape and function of the tooth after endodontic treatment are the following:
- Dental filling. This is the most common method of tooth restoration. After the root canal treatment, the tooth can be restored with a filling when:
- The tooth crown is not severely damaged.
- The patient chooses to refuse or delay dental prosthetics.
In many cases of root canal treatment, a dental filling is not considered to be the most reliable method of tooth restoration.
- Overlay. Overlays can be installed when the tooth’s crown is damaged by no more than 50% and only if the enamel is preserved along the entire periphery of the cavity (it is possible to connect the edge of the inserted overlay and the preserved edge of the enamel).
- Crown. The most common method of restoration after endodontic treatment. The main advantage of crowns is that they cover the entire surface of the tooth, thereby ‘sealing’ it in a way that neither microbes nor saliva, are able to get under the crown meaning tooth decay should not develop.
Endodontic treatment with dental microscope

Root canal treatment is a complex procedure that requires a high level of professionalism and precision. Errors in the treatment and filling of the root canals can lead to relapse and various infectious complications.
This is why the use of the dental microscope has become a breakthrough in endodontic practices. The quality and effectiveness of a microscopic treatment of tooth root canals is far superior when compared to traditional treatment methods.
Our clinic’s surgical microscope is capable of magnifying the image up to 30 times, allowing the endodontist to clearly see the treatment area and perform actions precisely.
Which is better – to treat infected dental canals or get an implant?
Endodontic treatment allows the preservation of natural tooth tissues. However, it is important to evaluate: the extent of bone damage on the treated tooth; the level of tooth mobility; the number of cysts/granulomas on the tooth root. All of this can determine the duration and effectiveness of treatment.
Teeth implantation is one of the most advanced and modern ways to restore dental functionality and aesthetics. Its disadvantages are the relatively high cost of materials and services, as well as the need for the natural tooth to be extracted.
The selection of the optimal method for your specific clinical situation is an important topic, which is to be discussed during the consultation with the dentist. However, the choice of the most effective method always depends on the condition of the tooth (canals, bone tissues, and gums), the number of missing teeth, the general health of the patient, and many other personalised factors.
Endodontic treatment in our clinic
Endodontic treatment in our clinic is performed by highly qualified specialists who have many years of experience. Extensive knowledge of innovative diagnostic methods and treatment options and an attentive and responsible approach to the treatment of each patient – these are the values that guide our dentists.
To ensure the comfort of our clients, all procedures are performed carefully and painlessly. Only the highest quality dental material and modern equipment are used during the treatment.
This allows us to efficiently perform even the most complex endodontic surgeries. Even in severe clinical cases, we aim to maximise the preservation and restoration of our patient’s teeth, health, and smile.
Pricelist
Adults
| Analgesia | 15 € |
| Periapical X-ray | 20 € |
| Temporary dental filling | 20 € |
| Injection/replacement of calcium substance | 20 € |
| Removal of endodontic pin | 100 € |
| Removal of fractured endodontic instrument parts | 100 € |
| Root canal access formation | 65 € |
| Accessing the tooth root canal | 65 € |
| Filling of a tooth root canal | 65 € |
| MTA application | 65 € |
| Preparation of the crown for the overlay when the re-treatment is not required | 65 € |
| Revision | 50 € |
| Disposable materials | 30 € |
| Single root canal treatment and filling with general anaesthesia | 200 € |
Children
| Treatment of milky tooth pulpitis with analgesia | 120-140 € |
| Treatment of milky tooth pulpitis with sedation | 150-180 € |
| Treatment of milky tooth pulpitis with general anaesthesia | 175 € |
| Treatment of pulpitis using MTA cement | 170 € |
| Single root canal treatment and filling | 200 € |