Pulpitis – inflammation of the tooth nerve
Dental pulp is the soft living part within every tooth which houses the blood cells and nerves for that tooth. Pulpitis occurs when the pulp becomes inflamed, often due to bacteria passing through a crack in the hard outer layer known as enamel.
If left long enough pulpitis becomes irreversible and the only treatments are a root canal, the removal of all the pulp, or pulling the tooth entirely.
Visiting your dentist as soon as you spot signs of pulpitis can be an important factor in the progression from reversible to irreversible pulpitis.
What is dental pulp?
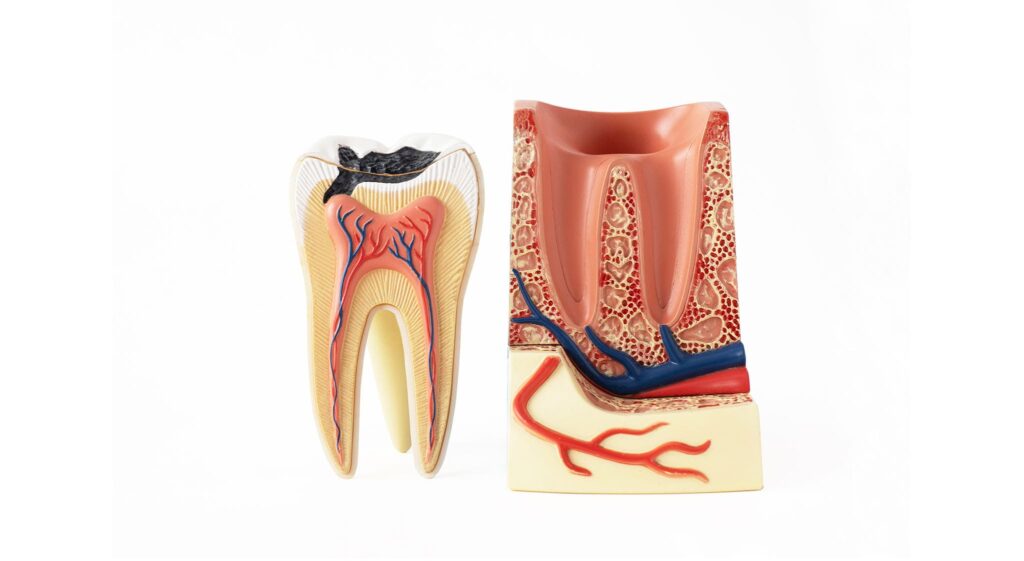
A tooth is structured in a series of layers, each with its function and properties.
The crown of the tooth is covered in a hard protective layer known as enamel, composed of the mineral calcium phosphate. Enamel is thought to be the hardest tissue found in the human body. Enamel protects the softer underlying layers and acts as the abrasive surface during chewing.
Beneath the enamel is a comparatively softer, but still hard material known as dentine. Dentine provides structure and support to the tooth while also being porous, which allows sensations to be passed down to the inner layers which contain the nerves. Dentine is what provides the natural colour to your teeth since enamel is transparent. However the enamel can become stained which can darken the already slightly yellow colour of dentine. Since dentine is porous it can become an easy avenue for bacteria to traverse to the softer more sensitive layer known as pulp. Therefore it is important that the enamel remains intact and does not become damaged, revealing and exposing the dentine.
The deepest and most secure layer of the tooth is the pulp. The dental pulp is composed of blood vessels, connective tissue, nerves, and specialised stem cells. Stem cells are a type of cell that is less specific than a regular cell. Stem cells have the potential to divide and become specialised cells, cells which have a specific job within the body. This means stem cells are important in maintaining the health of the body and in this case the teeth. The stem cells within the tooth specifically produce dentin, which if damaged is replaced, while the enamel cannot be repaired by stem cells.
The pulp aids the regeneration and health of the tooth by providing nutrition, which is brought into the tooth via the blood vessels. If the pulp becomes damaged then the tooth loses its nutrient supply, as well as nerves becoming damaged, which can lead to the tooth starting to decay and rot.
Pulpitis causes, diagnosis, symptoms and treatment

Pulpitis is the inflammation of the dental pulp within the tooth. This can be a very painful experience due to the nerve endings found within the pulp.
There are two main types of pulpitis, reversible pulpitis and irreversible pulpitis:
Reversible Pulpitis – The earlier stage of pulpitis, often has few symptoms except for sharp bursts of sensitivity and a moderate level of toothache. This limited level of inflammation can be reversed as it has yet to irreparably damage the pulp. Pain will be felt when a stimulus, often cold or sweet, comes in contact with the tooth. The pain will be sharp and moderately painful but will subside in several seconds upon removal of the instigating stimulus.
Irreversible Pulpitis – The later and more serious stage of pulpitis. This occurs when the inflammation has progressed and the pulp has started to die. This can cause spontaneous bursts of pain, and when stimulus (cold or sweet) are applied the pain will last for minutes or longer before subsiding. The pain may be difficult to pinpoint to just a specific tooth, with the pain often being felt across multiple teeth in both the top and bottom arches. Once the pulpitis progresses even further the tooth may no longer be sensitive to stimulus, this is due to pulpal necrosis causing the nerves to begin to die. As infection progresses abscesses can cause the tooth to separate from its socket and feel out of place within the mouth. As the infection spreads you will likely start to develop fever and other infection symptoms.
Causes of pulpitis
- Cracked tooth – A fracture in the enamel of the tooth exposes the porous dentine and opens up an avenue for bacteria to pass downward into the pulp. A cracked tooth can come from several causes, such as biting something hard, opening packaging using your teeth, or a physical injury to the tooth (such as a sporting injury)
- Bruxism – Excessive grinding and clenching of the jaw. Often found in patients with TMJ disorder (temporomandibular joint disorder) or those suffering from anxiety. This causes the enamel to become cracked or wear away.
- Cavities (Caries) – Often caused by poor dental hygiene, mixed with excess sugar and pockets of bacteria. This causes deep holes of decay within the tooth. These holes can create a pathway for bacteria to reach the inner pulp leading to infection and pulpitis.
- Malocclusion – A bad bite. This puts excess stress and wear on specific teeth leading to the enamel being worn down and damaged.
- Dental procedures – Your pulp can also become inflamed during specific dental procedures, though it is rather rare. For example, a filling can cause the pulp to become inflamed due to the heat used in setting the filling. Poor hygiene during a procedure can also lead to bacteria entering the pulp. This is something we take seriously at our clinic and we take the utmost measures to reduce the chances of this occurring.

Treatment for pulpitis
Reversible pulpitis is, as the name suggests, reversible. To reverse reversible pulpitis it is necessary to treat any underlying conditions that may be causing this. This usually involves the removal of tooth decay, performing any fillings that may be needed, or replacing the cracked and damaged crown with an artificial replacement crown. Antibiotics are often used if the inflammation is due to an infection within the tooth, though if the infection is present it is getting dangerously close to progressing to irreversible pulpitis.
Irreversible Pulpitis is, despite the name, somewhat “reversible”. While the pulp may have become irreversibly damaged, the tooth itself can still often be saved. Through a process known as a root canal, the dead and infected pulp is removed and replaced with an artificial filler. The blood supply to the ligaments that hold the tooth in place is usually preserved, with just the nerves and infection being removed. This will prevent future decay and also the pain you will be experiencing. If the infection has progressed too far, the tooth may have to be extracted. This is a last resort however and only for the most extreme of circumstances.
Root Canal Procedure
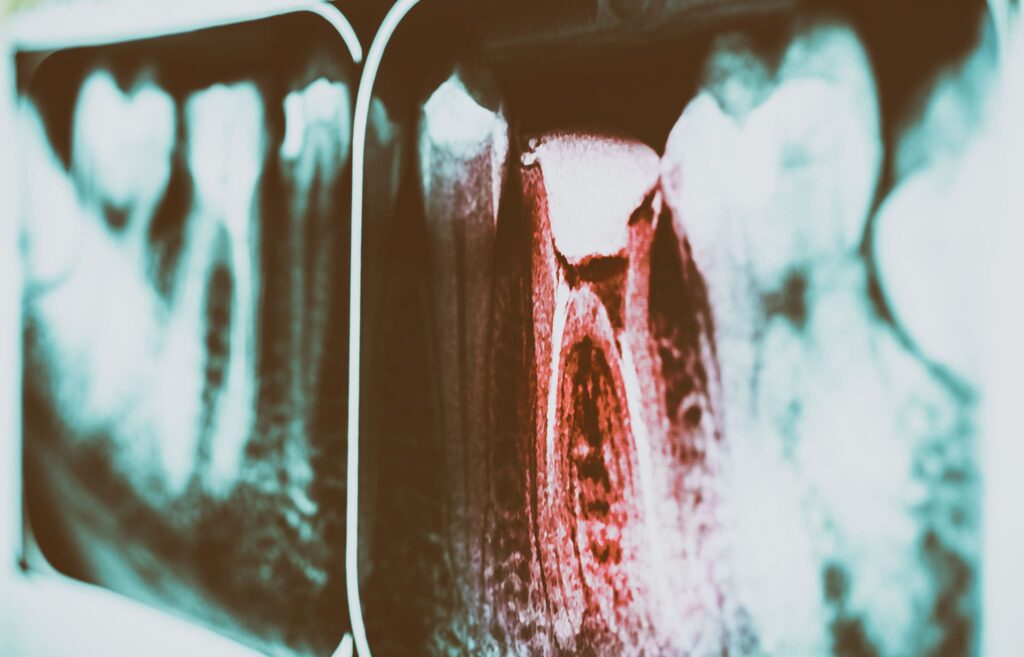
Root canals are usually performed over 2 or more procedures. Before the first procedure, you will likely have a series of x-rays and other scans performed to build a better understanding of the problem.
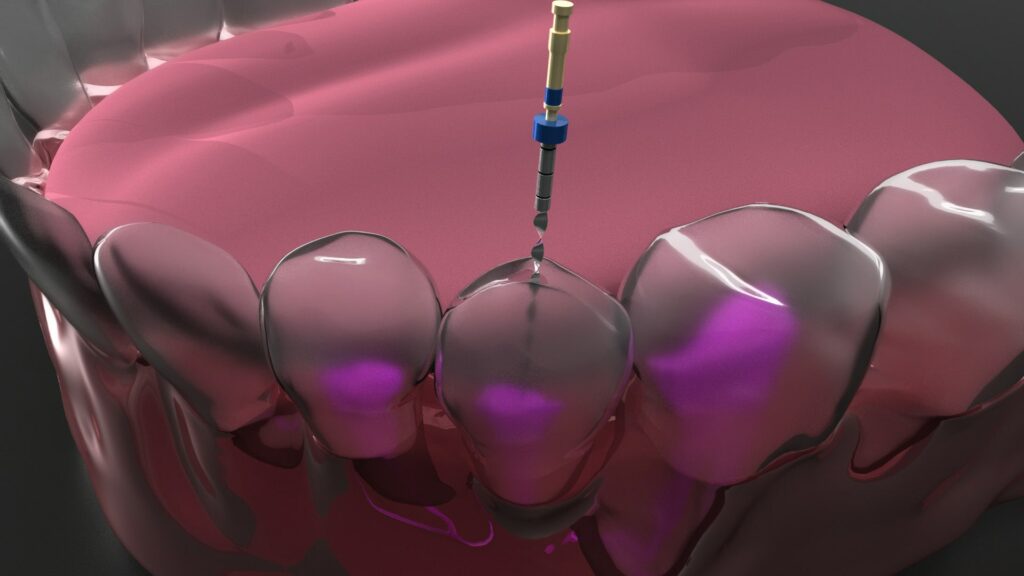
After cleaning and securing the tooth, the dentist will apply the chosen anaesthesia to the tooth. Usually, only local anaesthesia is required, however in cases where the patient struggles to handle the procedure then sedation may be used.
After the tooth is fully numb, the surgeon will use a drill to open the crown of the tooth. This allows the surgeon access to the softer pulp beneath. The pulp is then removed using a tool known as a file. All the pathways (canals) in the tooth are cleared down to the roots.
Depending on the severity of the infection, the dentist may choose to apply a topical antibiotic within the cavity to ensure that the infection is gone and the bacteria do not re-infect the healing tooth.
Once the tooth has been fully cleared, a biocompatible material is used to fill the canal within the tooth. The most commonly used material is gutta-percha, a rubber-like sealant. This is then capped with a temporary filling, to prevent saliva and bacteria re-entering the tooth while it sets. The reason a permanent filling isn’t used initially is to allow a few days to pass to check to see if any infection remains. Once this has been confirmed you will visit the clinic for the final procedure where the temporary filling is replaced with a permanent one.
Since the pulp is removed, the dentin is no longer able to be repaired so your teeth will become more fragile compared to before the procedure. Therefore the dentist may suggest having an artificial crown added over the top of the real tooth and increase its durability and strength. The crown dramatically increases the survival rate of the tooth post-operation and, assuming you look after the tooth it can last well over a decade post-procedure.

Why should pulpitis not be left untreated?
Just like any other infection, pulpitis has several complications if left untreated. The infection may spread into the bone or soft tissues around the tooth causing a periapical abscess (dental abscess). If the infection continues to spread it can lead to a condition called cellulitis, or the infection of the skin. This can be life-threatening and can lead to changes in both mental state and physical.
Prevention of pulpitis
The prevention of pulpitis involves many of the same preventative methods as most other dental ailments. The risk of pulpitis and many other dental ailments can be reduced significantly by practising good oral hygiene and visiting your dentist regularly. Your dentist will be able to spot the warning signs of pulpitis and can advise you on what to do next. Having a routine professional oral cleaning appointment can help reduce the risk of caries by removing plaque and tartar.
Reducing your intake of sweet and acidic foods, such as cola and candy, can massively reduce the damage your teeth can sustain.
Treatment of bruxism via the use of a splint or tooth guard can protect your teeth, especially if you grind while sleeping.
Visiting your dentist as soon as you spot signs of pulpitis can be an important factor in the progression from reversible to irreversible pulpitis.
Treatment of pulpitis in our dental clinic
Our dentists are all expertly trained and each has many years of experience in performing all sorts of procedures. Since the treatment of pulpitis and root canals are so common they all have plenty of experience treating this specific condition.
We provide our dentists with all the best equipment, including a new cutting-edge dental microscope, which allows our dentists to use their expertise to achieve the best possible result.
If you have any signs or symptoms of pulpitis, other dental conditions, pains, or concerns, then do not hesitate to contact our clinic.